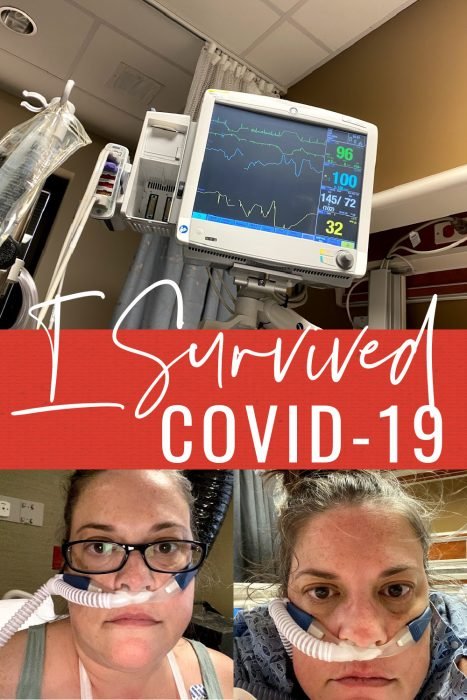
I survived COVID-19
This was originally written in 2020 before the COVID vaccines were available. I survived COVID-19 after a 12-day hospital stay, including time in the ICU. As the Delta variant is ramping up and ravaging the country, I want to share my story again. I hope my story can help others who are hospitalized themselves or who have loved ones who are, and can encourage you to get vaccinated to avoid going through what I did.
I thought I was going to die.
I am a bit of a hypochondriac, but I was not even exaggerating. I was laying on the bathroom floor where I had fallen after fainting, sore from hitting the bathtub on my way down. I called my mom.
“Mom? Am I going to die?”
Then, I told her I was heading to the hospital. After 4 days of battling COVID-19 and a high fever at home, and with my O2 below 90, I knew I needed care.

Being Admitted
My husband dropped me off at the hospital. He couldn’t go in with me. So, I gave him a hug and told him I’d see him soon. Little did I know, soon would be almost 2 weeks later.
I didn’t wait long in the ER at all. I figured they would give me some supplemental oxygen to get my O2 level back up and send me home. They put me on oxygen for a while, but my oxygen level stayed low. I needed high flow oxygen, which they couldn’t do in the ER, so they admitted me.
There’s nothing like being told you’re being admitted to the hospital because you have low oxygen and being totally alone. It was terrifying.
I had to wait a while for a room. When I was moved, I was hooked up to the high flow oxygen unit. The tubing was so much bigger than a regular nasal cannula, and it was so loud. But, I was feeling good. My fever had broken, and I felt like I was better. I knew I wouldn’t be there long.

Moving on Up….To the ICU
When the pulmonologist came to see me, she told me she wanted me to be moved to the ICU. I’m sure she saw the fear in my eyes, because she assured me it was because the nurses there have only 2 patients each, so they can give more care than those on the floor. OK. Cool. So, I was going to be fine. I wasn’t really that sick.
And then, she brought up life support. Just in case. Cue the fear all over again. The thought of being put on a ventilator scared me. What if I didn’t heal and didn’t make it? There were so many thoughts running through my mind, and I had no one there with me to handle it.
I was still fairly calm as they wheeled me upstairs to the ICU. But, when I arrived, there was a crazy amount of activity. Three nurses were waiting for me. They transferred me to the bed, and then I had to be completely wiped down with antibacterial wipes before I changed into my gown.
I already had an IV in from the ER, but I had to have a second one as part of the ICU rules – just in case one stopped working. They had already told me the protocol – I would be receiving plasma, Remdesivir and Dexamethasone. I figured I would start treatment in the morning, but no – they were already on their way to pick up my bags of plasma to begin immediately. I felt comfort in the fact that they were being so proactive and starting everything right away. Maybe I would be OK.
That night, I received 2 bags of plasma and my first of 5 doses of Remdesivir. It was all pretty fascinating and neat to watch as it went into my body.
Settling Into ICU Life
The ICU was really hard on me mentally and emotionally. I wasn’t allowed to eat anything but clear liquids until my my oxygen was lowered to 50L just in case they needed to intubate me. The thought of that terrified me. I was so grateful to have a nurse who noticed me crying in the middle of the night and came in to sit with me and talk me through it. Everything was so overwhelming, and he told me I needed to fight to keep myself off the ventilator. I was determined that was going to be my goal.
I was very sick – more than I realized. Listening now to voice memos I recorded while I was in ICU, I can hear how terrible I sounded. Friends told me they could tell I wasn’t well by my messages to them. My mom and husband told me I was very, very sick. I thought I was fine the entire time.
When I was admitted, I was on 80L of oxygen. I thought that was normal but now, as I see the levels other patients are at and am told that those are high amounts, I realize why my primary care doctor was so shocked that I was still alive. They told me I didn’t have a lot of wiggle room before I would need a BIPAP mask, so I knew I had to work hard to bring my oxygen level down. BIPAP is one step before the vent. My goal was to reach 50L because at that point, I could start to have solid food, which meant I was out of the woods of needing a vent – a major goal.

How could I fight COVID? By proning – laying on my stomach to open up the back of my lungs and let air in. My goal was to prone for 5-6 hours a day plus all night long. After breakfast – broth, Jell-O cubes and Italian ice – I would wait about an hour and then flip onto my stomach. And, that was where I would stay until lunch – another meal of broth, Jell-O cubes and Italian ice. Proning was exhausting. It wasn’t comfortable, and my head ended up having to lay on the tubing, so all I heard was the LOUD whoosh, whoosh of the oxygen. I tried to watch TV, but I ended up sleeping most of the time. That’s OK, though, because sleep was another vital part of recovery.

My New Routine
I settled into a new routine. In the mornings, I was woken up around 6 a.m. for blood gas draws. They had to draw blood from the artery in my wrist to get the exact amount of oxygen and carbon dioxide in my blood. The normal level is 75-100, and mine was 52.9 when I was admitted, which they said was critically low. I also had a blood gas drawn in the afternoons. I’m not going to lie – it hurt. A lot. My wrists were SO bruised and battered. When I video chatted with my daughter, she asked me who I fought. The needle, and the needle won.

I had my 3 meals of broth, Jell-O and Italian ice. In the evenings, I would get an extra Italian ice or some ice cream as a treat. In between my meals, I would prone. And, I used my spirometer throughout the day to exercise my lungs, and respiratory came by every 4 hours to do my inhalers. After dinner, I would sit up for a bit and watch TV before the nighttime routine.
It was hard to get used to nighttime and really having no shame. I had to use a beside commode, and I had to have a nurse in the room when I went to the bathroom. I didn’t have the energy to go more than 2 steps from the bed. My O2 sats would plummet, and I felt like I was suffocating when I used the bathroom. I was terrified every single time. It would take me a bit after getting back in bed to get my sats back up. And, every night, I had to have a sponge bath, have my sheets changed and get a new gown. I hated it. I dreaded when 9 p.m. rolled around.

I spent a lot of time watching my vitals, too – so much so that my nurses and respiratory therapists told me to stop! It was hard not to watch them, though, because I knew my oxygen level needed to stay in the 90s to be able to move the amount I was being given down.

Within a few days, I made it to 50L of oxygen. Y’all, I have NEVER been so happy in my life to EAT – even hospital food. And, really, the food there was not bad at all. My first meal was pasta, broccoli and a breadstick and even though it was cold, it was the best pasta I had ever had.
The really interesting thing about being a COVID patient is that nothing was allowed to leave my room with the exception of food trays. One day, my Italian ice melted before I finished my meal, so I asked if they could refreeze it. I was told they couldn’t take it out, so they had to throw it away and bring me a fresh one.
I also really loved that I had one nurse for almost my entire ICU stay. She was great, got me everything I needed or wanted, and it was enjoyable to talk to her. It was strange only interacting with a few people every day.

Moving Out to the Floor
After 6 days in the ICU, I was able to wean off high flow oxygen and use a regular nasal cannula. That meant I could move to the floor! I have never been so excited in my life. I had gone from 80L of oxygen to 5L. That is a HUGE jump in less than a week. I was so excited to get the heck out of dodge and onto the floor, but it was kind of sad leaving the staff that I had come to know so well.
When I got to my new room, my nurse and tech got me settled and then asked me if I wanted anything to eat. Did I?? I was on a limited diet in the ICU, and I was starving, so I devoured the graham crackers and peanut butter they gave me.
My first thoughts when I moved to my new room was that I had done it. I had gotten out of the ICU without being put on BIPAP or on a vent. But, it was strange not being hooked up to a vitals monitor 24/7. I didn’t know what my oxygen level was at until they came in a few times a day to check. The unknown drove me nuts! But, I continued my proning – though I did it now on my side rather than my back – and using my spirometer.

Taking a Mental Toll
There were so many ups and downs both in the ICU and on the floor. I would have my oxygen level lowered but then would need to be moved back up because my levels weren’t staying where they needed to. I learned to do deep breathing to help my levels stay up. In slowly through my nose and out even slower through my mouth. I realized how much I actually breath through my mouth when I needed to do it through my nose!
What really started to get to my was the isolation. I only saw my nurse, respiratory therapist and doctor. No visitors are allowed on the COVID floor. It was really hard on me emotionally. Yes, I video chatted with my family several times a day, but it wasn’t the same. I had many cry sessions because I missed people. I missed my family.
It was also really hard feeling like I had the plague. Everyone had to dress in a gown, wear two masks and a shield or goggles to come into my room. I wasn’t allowed to leave and go into the hall.

Since there was nothing to do, I realized I started tracking my day in blocks. At 6 a.m., I was woken up for blood work. I would scroll Facebook and watch Amazon Prime on my phone until breakfast around 8:30 a.m. After breakfast, I knew I had 4 hours until lunch. I would usually take a nap because I was tired from being up at 6 a.m., and then I would watch HGTV. After lunch, I had 4 hours until dinner. I would video chat with my family and either watch HGTV or Amazon Prime on my phone, all while proning on my side.
After dinner, I had until around 9 or 9:30 p.m. when the night nurse rounded for vitals and medicine. If it was a night Big Brother was on, my husband and I would watch together. On Saturday night, my husband dropped off a bowl of popcorn, and we had family movie night with them watching at home and me at the hospital.
On Sept. 25 – 8 days after being admitted – I had my first 6 minute walk. In order to go home, I had to be able to walk for 6 minutes with no more than 2L of oxygen. I had to use 4L. I was so disappointed. I was so ready to go home, but my body wasn’t ready. I needed to stay, but it was so, so hard. I’d already been gone so long. I knew I needed to work hard for my next walk so I would pass it.

I tried my walk again on Monday, Sept. 28, and I was told I did it with 1L of oxygen. That meant I passed! I could go home! The respiratory therapist told me she would tell the doctor. She wasn’t sure if I would go home that night or the next day. I was SO EXCITED. I was going to see my family!
The next day, I was pretty impatient. I was on day 12 in isolation in the hospital and SO excited to see my family. I didn’t even really pay attention to the fact that respiratory didn’t make their morning rounds. The pulmonologist usually rounded between 2-3 p.m., so I was watching the clock. That time frame came and went, and the doctor didn’t come by. Around 4 p.m., I called the nurse and my husband started calling. She didn’t know why no one had been by but she would find out.
My nurse came in and told me she had looked up my walk test results and I had failed by needing 3L of oxygen. No. That was not what I was told. I had done a good bit of it on room air and only needed 1L to complete it. At that point, I lost it and broke down. I was done emotionally. I needed to see my family. The charge nurse came in, and I tearfully told her what I had been told about my walk test. She assured me the pulmonologist would be down soon to talk to me.
Around 5 p.m., the doctor finally rounded. She told me again that I had failed. But, I had been told I had passed! They had even said they weren’t sure if I would go home the night before or the next day. That’s not what my chart said. Y’all – frustrated doesn’t even BEGIN to describe how I felt. It was a miscommunication, but it was a BIG one, and it was NOT OK.
We could try the test again. If I passed, she would sign off on my discharge. I was defeated at this point. If I had been told I had passed but actually hadn’t, how would I pass it now? The respiratory therapist came and got me ready. With the pulse ox on my finger, I got up to walk. This time, I got to walk the hallway. I hadn’t seen the outside of my room in almost 2 weeks except for the trip there from ICU. There were PEOPLE. Then, I saw my very first nurse I had on the floor, and she was clapping for me. I had tears streaming down my cheeks. I felt like I was SO CLOSE to going home yet so far. I kept my eye on my pulse ox. It dropped to 89 and then to 88. They turned my oxygen on to pulse so it would only come on when I breathed through my nose. My oxygen level bounced around but ended up in the 90s. I had passed! I was going home!

The Longest Wait
Waiting to be discharged seemed so much longer than the time I had spent in the hospital. They needed to set up my oxygen at the house before I could be released. Since my daughter had dance, we had to have it set up after her class. I ate my last meal at the hospital and tried to distract myself by watching TV. My nurse came in, took out my IVs and told me I could get dressed to go. I got a text from my daughter. “I’m crying!!” Me, too, kiddo. Me, too. When my husband arrived, I got my discharge instructions with 3 doctors appointments in the next two weeks, and loaded up all my stuff. It was the longest wheelchair ride ever. But in just a few minutes, I was outside hugging my family. I hadn’t seen them in almost 2 weeks. Tears were streaming down all of our faces. I told them I was never letting them go.







Leave a Reply